Laerdal has been involved in helping save the lives of infants and babies in HICs for more than half a century. It is only relatively recently that significant efforts have been directed to LMICs and included the health of the mother as well. The lessons learned from this, with the imperative to develop solutions that were highly cost effective and improved the efficiency of the limited pool of nurses and midwives, can also be translated to HICs where both human and financial resources are being increasingly stretched.
It was in the mid-1960s that Laerdal introduced its first baby, Resusci Baby. The AHA guidelines for neonatal resuscitation were published in 1980 with support from the company. SimBaby, a high-fidelity simulator first introduced in 2003 and recently updated, continues to serve the needs of the AHA Pediatric Advanced Life Support course.
In addition, an alliance with the UK Bristol-based company, Limbs & Things, over many years has supported skills training and higher-fidelity birthing simulation.
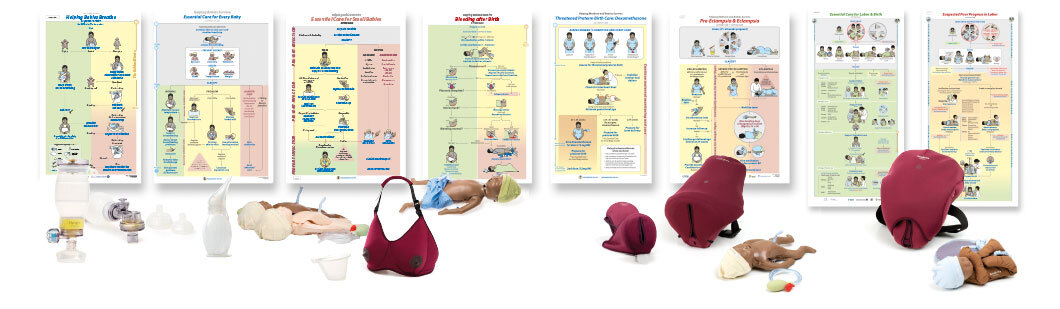
Laerdal’s involvement in neonatal well-being has accelerated over the last three decades in its close partnership with the American Academy of Pediatrics and its Neonatal Resuscitation Program (NRP) which was launched in 1987. The program is now used in 130 countries with over 200,000 instructors and over 4 million providers trained. SimNewB, first introduced in 2008 with the second generation following in 2019, and Premature Anne were designed especially for this program. And it was this involvement with the NRP that stimulated the formation of LGH.
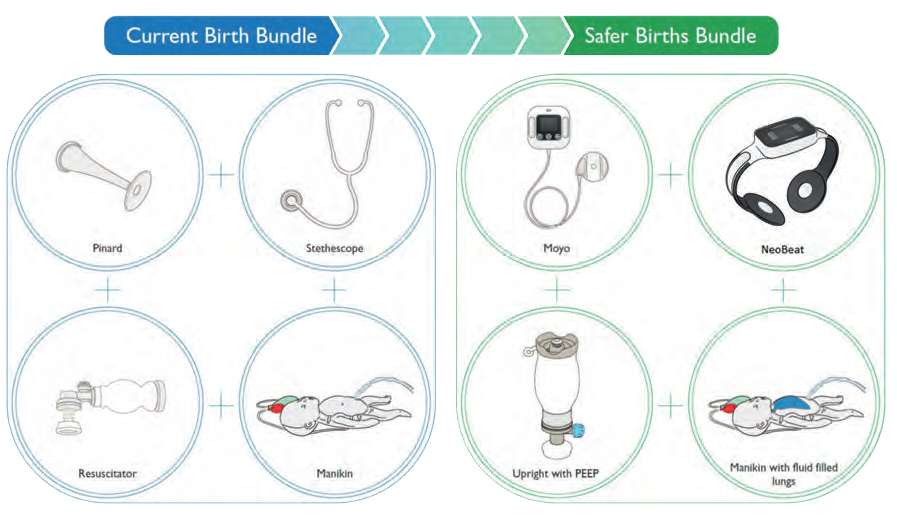
A prime example of how solutions originally designed for low resource settings can serve the needs of HICs is the NeoBeat newborn heart rate monitor. This innovation was developed to support the Helping Babies Breathe (HBB) program. Supported by the WHO and the Gates Foundation, researchers have validated the NeoBeat at a network of hospitals in Europe and Australia, comparing its efficiency during real resuscitation with traditional tools. It has generated such great interest in those validation sites that they want to use it themselves. They find that this simple, low-cost pulse monitor provides heart rate data much quicker than their pulse oximeters and is much easier to apply to a newborn than traditional ECG electrodes, enabling lifesaving ventilation to be started sooner.